When news came through late last week that cystic fibrosis drug Trikafta was approved for sale in Canada, Kelly Murphy says she felt a sense of relief.
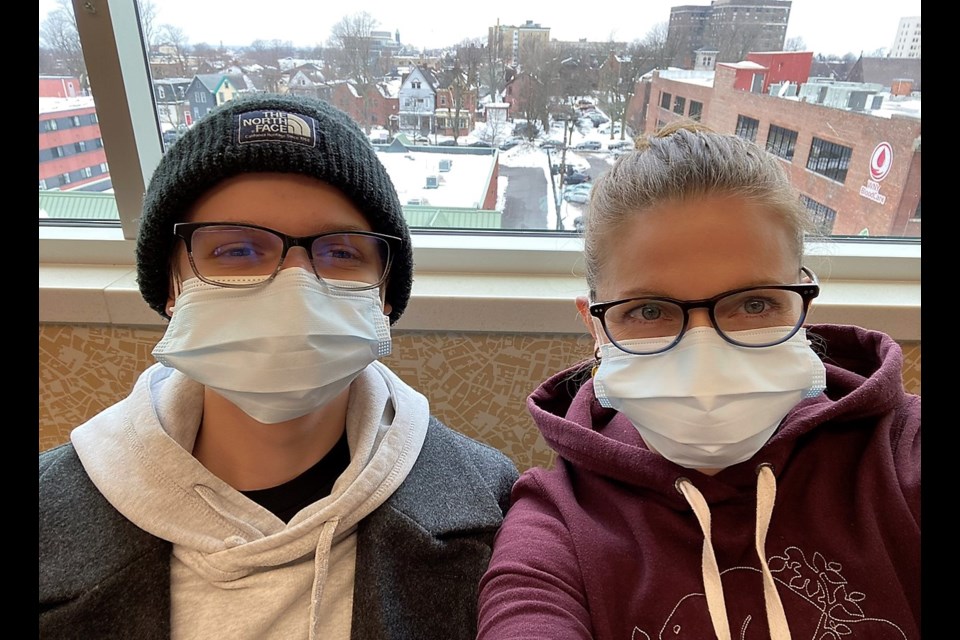
The Collingwood mom has been a long-time advocate for Health Canada to approve the drug, after seeing her son Finn struggle with a cystic fibrosis (CF) diagnosis since he was born. Now Finn is 17 and through the help of an anonymous benefactor, Murphy was able to get the drug from the U.S. and has seen first-hand the wonders it is able to do for her son’s health.
“The unconscionable delay in access of this drug to our CF community truly lays bare our government’s inadequacies,” said Murphy. “Words can’t express the relief that comes with the news that our doctors can now simply prescribe life-saving medication.”
Finn was born with cystic fibrosis. He was resuscitated at birth at CGMH and rushed to Sick Kids. Since then, Murphy says Finn has spent more than 14 months of his life admitted to a hospital.
Cystic fibrosis is a progressive, genetic disease that causes persistent lung infections and limits the ability to breathe over time.
“His lungs were healthy when he was younger, but as time passed and the bacteria in his lungs became resistant to all available antibiotics, the frequency of hospital admissions and his burden of care increased,” said Murphy.
In 2020, Finn’s condition worsened with his lung function slipping as low as 39 per cent and averaging in the low 40s.
He was diagnosed with cystic fibrosis related diabetes in August 2020 and began using insulin.
“He had given up playing hockey two years before and by last fall had trouble going on an easy-going walk or climbing the stairs to his room. He was routinely coughing up blood from his lungs,” said Murphy.
Murphy says she felt heartbroken and enraged seeing miraculous stories of recovery and healing of those with CF in other countries who received Trikafta, knowing Health Canada was not approving the drug.
However in November, a glimmer of hope came along.
A benefactor came forward and offered to pay the cost of Trikafta for Finn if the family could find a doctor in the U.S. to prescribe it, which they did.
“In less than seven months on Trikafta, Finn has dropped his CF-related diabetes diagnosis and no longer requires insulin. He has not had one hospital admission during this time. He has stopped coughing all night. His appetite is huge! He has gained over 20 pounds and went from requiring tube feeding seven nights a week to just two and will likely be able to discontinue them altogether very soon,” said Murphy.
In addition to these improvements, Finn has also seen a decrease in needing daily chest physiotherapy, has discontinued use of two of his five inhaled medications. His lung function has increased to 62 per cent and is considered stable without antibiotics.
“Beyond all of these important changes and improvements there is this: my stoic teenager who was facing a death sentence has the spirit of a teenager once again,” said Murphy. “What a joy to see him participating in life with his lovely girlfriend out biking, hiking, swimming, and golfing. All of this is new and was impossible for him last summer. He was just hired for his first part-time job.”
“It’s unbelievable what Trikafta has done for him,” she said.
Now, Murphy said her attention is turned to next steps, which include advocating for publicly funded access to the drug.
“I’m applying for (and probably fighting) my insurance company to pay for Trikafta, but what of those without private insurance?” said Murphy. “We can’t rest yet.”
Currently, the drug is approved by Health Canada for use in individuals 12 and older. Murphy said she would like to see Trikafta approved for children six and up. As cystic fibrosis ravages lungs over time, she says earlier interventions would make a huge difference.
“These children can grow up planning their futures instead of wondering how long their bodies will hold out and thinking existential thoughts such as ‘what’s the point’ -- a frequent and depressing expression of Finn’s in recent years,” said Murphy.
“Now, he can see the point and is preparing in earnest for a real future.”